

- #Aim specialty health prior auth form how to
- #Aim specialty health prior auth form verification
- #Aim specialty health prior auth form code
Learn how to check authorization information in ProviderOne. Step 5: Check the status of an authorization or retrieve correspondence Barcode cover sheet for pharmacy PA requestsįor step-by-step instructions: view our guide for adding supporting documents to an existing request in pend or approve/hold status.
Barcode cover sheet for general PA requests.
#Aim specialty health prior auth form code
Use one of the following cover sheets when submitting supporting documents to an already existing authorization: For example, when responding to a pend for additional information, or an existing approved authorization requires a billing code or NPI update. Submit supporting documentation to an existing authorization There is a cost associated which will be explained by Vyne Dental.

Note: The General Information for Authorization form (13-835) must be typed and be page 1 of your fax to avoid delays.
#Aim specialty health prior auth form verification
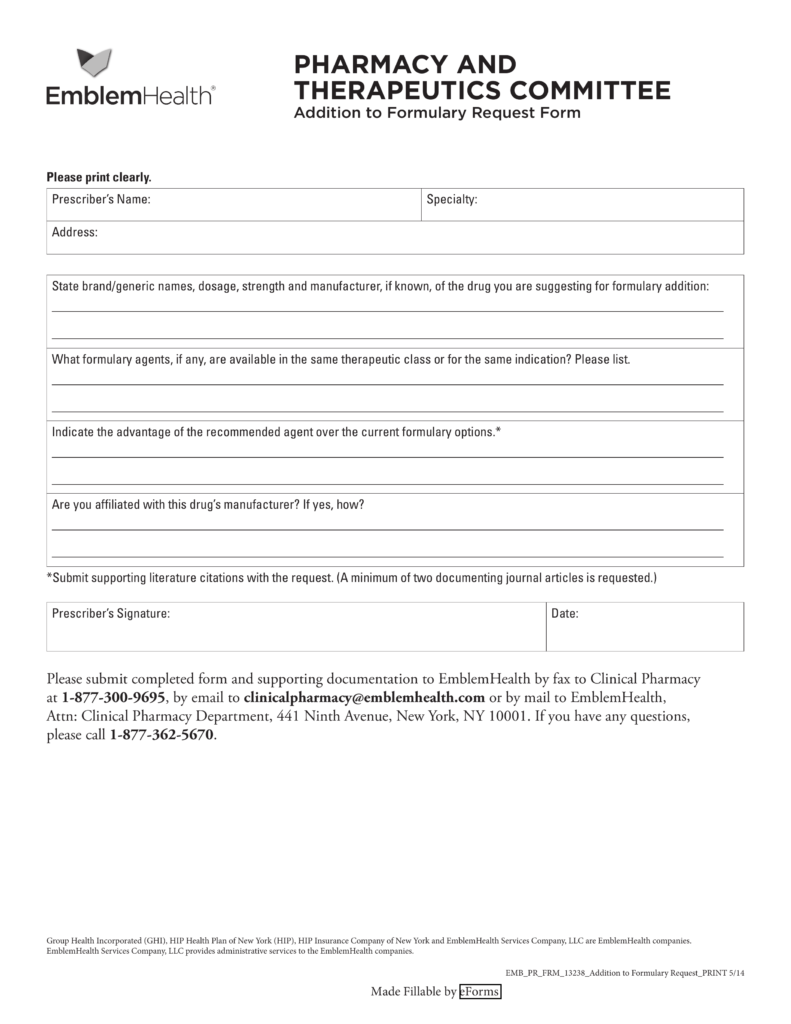
Upon successful submission, a provider will receive a 9-digit reference number the reference number is verification that the agency has received your request. This feature includes the ability to attach records, color photos, and x-rays. Providers can direct data enter authorization requests directly into the ProviderOne System. By direct data entry (DDE) in the ProviderOne portal Please submit by direct data entry or by fax. Submit by mail not available at this time: The agency is no longer accepting prior authorizations requests or supporting documentation by mail. Pharmacy Information Authorization (13-835A).General Information for Authorization (13-835).One of the following forms is required to initiate the prior authorization process. View a list of all prior authorization forms on our Forms and publications webpage. Step 3: Find and complete formsĪll services or items requiring prior authorization must be submitted on the General Information for Authorization (form 13-835), each individual service or item may require additional forms. Physician-related/professional servicesįor a complete list, visit our Provider billing guides and fee schedules webpage.Note: All codes on this fee schedule require prior authorization Complex Rehabilitation Technology (CRT).
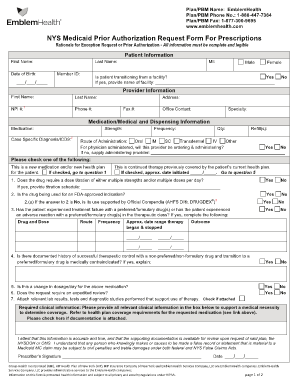
The following is a shortened list of regularly used billing guides and fee schedules. See whether a PA is required for that place of service.Make sure that it is covered for the location where you are performing the service, and.For example: Check the physician fee schedule and the ambulatory surgery center (ASC) fee schedule if you are performing the service in an ASC to: You may have to check multiple schedules or guides based on place of service. Important: Check the code or service in the fee schedule and provider guide for where the services will be performed.


 0 kommentar(er)
0 kommentar(er)
